Overdose Prevention & Response
Crisis & Help Lines in Massachusetts
The Massachusetts Behavioral Health Help Line (BHHL) is a clinical hotline staffed by trained providers and peer coaches offering clinical assessment, treatment referrals, and crisis triage. Call or text (833) 733-2445 or chat here.
The Massachusetts Overdose Prevention Helpline is staffed by harm reductionists and people with lived and living experience with overdose. It connects people using drugs to trained operators who can call for help.
Veteran Overdose Deaths in Massachusetts
The Massachusetts Injury Surveillance Program publishes data on drug overdose and poisoning deaths within the state.
Veterans made up 12 percent of the 72,018 Massachusetts residents who experienced one or more of the 133,295 documented nonfatal overdoses from 2013 to 2021 (over 8,640 veterans).
In 2019, the Massachusetts Military and Veteran Drug Overdose Deaths data sheet identified 90 overdose deaths (along with 67 suicide deaths), with most involving multiple substances:
92 percent involved opioids (compared to 15 percent of suicides in 2019);
59 percent had 2–5 substances and 27 percent had more than five substances;
47 percent involved cocaine; and
37 percent involved alcohol (compared to 29 percent of suicides in 2019).
Veterans with fatal overdoses in 2019 were just over age 50 on average––almost 10 years older than non-veterans. Around 43 percent had a known mental health condition (compared to 52 percent of veterans who died by suicide). Veterans who overdosed were more likely to have been diagnosed with PTSD, to have alcohol involved, and to die at home compared to non-veterans.
Massachusetts Military & Veteran Overdose Trends
The only year data has been published specifically about military and veteran fatal overdoses was in 2019, when there were 90 overdose deaths and 67 suicide deaths. Over 8,640 veterans have had a nonfatal overdose from 2013 to 2021. Based on the total number of deaths there have been an average of around 960 nonfatal overdoses a year.
-
The Massachusetts Department of Public Health’s August 2017 Assessment of Fatal and Nonfatal Opioid Overdoses in Massachusetts includes information about veterans who overdosed. From 2011 to 2015, the percentage of veterans with a fatal opioid overdose was three times the average.
One significant data gap identified in the assessment of public health data available from 2011 to 2015 to better understand the factors involved in overdose deaths was due to the lack of VA participation in the state’s Prescription Drug Monitoring Program, which was established in 1992.
(Although mandated reporting began in 2012, implementation and piloting began in 2015 and VA facilities in Massachusetts began utilizing PDMPs several years later; a nationwide interface was launched by the VA in 2021).
An analysis of the Massachusetts data from 2011 to 2015 demonstrated veterans were 69 percent more likely to experience a nonfatal opioid overdose and 132 percent more likely to fatally overdose compared to non-veterans. Another analyis demonstrated homeless veterans during this time were:
more likely to be men (80 percent) compared to nonveterans (62 percent), with women veterans overrepresented among homeless veterans in Massachusetts;
more likely to be over age 45 (77 percent) compared to nonveterans (48 percent); and
more likely to be receiving high dose opioid therapy (23 percent) compared to nonveterans (15 percent).
Homelessness and veteran status were independently associated with higher odds of fatal and nonfatal opioid overdose with a significant interaction between homelessness, veteran status, and risk of fatal overdose. The researchers recommended understanding health care utilization patterns to identify veterans’ treatment access points in order to mitigate risk by improving patient safety.
-
Veterans made up 12 percent of the 72,018 Massachusetts residents who experienced one or more of the 133,295 documented nonfatal overdoses from 2013 to 2021, with the percentage of veterans with a nonfatal overdose continuing at over three times the state average. This means an estimated 8,640 veterans in Massachusetts had at least one nonfatal overdose (an average of around 960 a year).
In total, 6,404 Massachusetts residents with a nonfatal overdose subsequently died by overdose. For every nine nonfatal opioid overdoses during this period, there was an average of one fatal overdose. Among all residents experiencing a nonfatal overdose:
77 percent were diagnosed with opioid use disorder (OUD) with
60 percent diagnosed before their first nonfatal overdose and
18 percent diagnosed following a nonfatal overdose;
72 percent were diagnosed with a mental health disability;
65 percent were diagnosed with a mobility disability;
55 percent had experienced homelessness since 2011;
47 percent had less than a high school education;
39 percent had experienced incarceration since 2011;
26 percent were diagnosed with a developmental disability;
21 percent were diagnosed with a vision disability; and
13 percent were diagnosed with a hearing disability.
-
The Public Health Data Warehouse links data from within the Department of Public Health and across state and county agencies to create a reliable population health database that informs policies and programs to reduce morbidity and mortality and keep people healthy.
The PHDW also designs/conducts studies to provide actionable recommendations to target resources to address public health priorities in Massachusetts and provides access to the data to enable researchers, academics, program planners, and others to address key issues and improve public health.
Community Advisory Board
The Department of Public Health’s Community Advisory Board (CAB) is led by the Office of Population Health, Special Analytic Projects Team, which manages the PHDW, which is an important source for data on military and veteran suicide and overdose trends. The CAB provides community perspectives to guide data collection and analysis in key areas.
Although veterans are not included among the “priority” populations, the CAB is comprised of key community stakeholders who are members of or work with BIPOC people, people with disabilities, substance use disorders, or mental illness, or who are experiencing homelessness or housing insecurity, are pregnant or post-partum, living in rural settings, or who have a history of incarceration, which all intersect with the veteran experience.
CAB members help DPH develop analytic questions for public health topics and priority populations; provide community member feedback and input and support the dissemination of results and information to the public. To learn more about the CAB or inquire about membership, email DPH.PHD@mass.gov.
Veterans are significantly more likely to experience fatal and nonfatal overdoses, particularly homeless veterans. There is insufficient data available for communities to implement effective suicide and overdose prevention strategies to mitigate risk factors within the veteran community. The percent of veterans with nonfatal overdoses has been over three times the state average since 2011.
US Military Overdose Trends
-
From 2017 to 2021, a total of 15,293 active duty service members experienced had overdoses. There were 332 fatal overdoses; around 7.5 percent were women.
Most fatal overdoses involved enlisted members (96 percent) under age 34 (80 percent).
Around 13.6 percent involved opioids only and 9 percent involved alcohol only, with the majority of overdoses involving multiple substances.
Only 12.7 percent of fatal overdoses were classified as suicides (42 suicide deaths).
There were 14,961 service members with nonfatal overdoses; around 32 percent were women. Around 42.4 percent of nonfatal overdoses were classified as intentional, which may reflect a population at high risk for future suicide attempts.
US Veteran Overdose Trends
-
Veteran drug overdose mortality, 2010–2019 examined the overdose deaths of 42,627 veterans nationally, including 18,573 with and 24,054 without recent VA healthcare use.
Overdose rates were higher for male veterans with recent VA healthcare in all years. The rate of increase in rates didn’t differ significantly based on recent access.
Overdose mortality rates increased faster among women veterans without recent VA healthcare and remained higher for women with recent VA healthcare access from 2010–2018.
Consistent with prior reports demonstrating higher opioid overdose mortality among VHA patients, the findings for 2010–2019 also illustrate the importance of implementing overdose prevention efforts, particularly among veteran men accessing VA healthcare with the greatest risk and among veterans not accessing VA healthcare, who have the most deaths.
Researchers analyzed national data on veterans in 2018 and 2019 and found that homeless veterans were more likely to receive risky and potentially inappropriate combinations of concurrent benzodiazepines and/or concurrent benzodiazepine and opioid or sedative prescriptions, increasing their risk of overdose.
From 2010 to 2019, 42,627 veterans died by overdose (along with the 65,547 veterans who died by suicide during that period). Veterans age 65+ had the largest relative increase in overdose mortality over time. The largest absolute and relative increases in overdose mortality rates during this time were in the Northeast region.
VA researchers found that mortality risk was greater for veterans with opioid use disorder who were not receiving buprenorphine compared to those who did across VA facilities from 2008 to 2017. Veterans without buprenorphine were over four times more likely to die by suicide or overdose, even after accounting for periods with methadone or naltrexone, and had higher all-cause mortality.
Access to Medication for Opioid Use Disorder
Despite strong evidence supporting the use of life-saving pharmacotherapy to treat opioid use disorder, there continue to be high levels of stigma surrounding Medication for Opioid Use Disorder (MOUD) among both patients and clinicians, particularly perpetuating the idea that patients are “substituting one drug for another,” among many other barriers to care.
-
Nearly half (46 percent) of the veterans with a fatal overdose in Massachusetts had a bystander present, which means there was an opportunity to intervene. It's important for veterans and their family members and caregivers to know what to do in an emergency. If you see someone exhibiting any of these symptoms, dial 911 immediately:
loss of consciousness or limp body
slowed breathing or choking
small, "pinpoint" pupils
pale, blue, or cold skin
slowed heart rate
Naloxone should be given to anyone showing signs of an opioid overdose; it has no effect on someone who doesn't have opioids in their system. A person experiencing an overdose will need someone else to give them Naloxone if it is available while waiting for first responders.
When used immediately after an opioid overdose, administration of Naloxone can rapidly reverse the overdose by temporarily blocking the effects of the opioids to prevent death.
Veterans who use opioids can ask their VA provider to prescribe naloxone at no cost.
Friends and family members of veterans and veterans who are not enrolled in VA healthcare in Massachusetts can click here to identify Naloxone and other harm reduction resources or contact their local pharmacy or health department to obtain Naloxone.
Eligible programs can obtain Naloxone through the Massachusetts Community Naloxone Program (CNP) to distribute to community bystanders.
-
MOUD is a first-line treatment available to veterans which may also be combined with counseling or therapy for veterans who need it. Buprenorphine is a partial opioid agonist that prevents/relieves opioid withdrawal symptoms and reduces cravings without the high associated with other opioids.
Risk Factors Involving Medications & Substances
In February 2023, a committee of the National Academies of Sciences, Engineering, and Medicine began a VA-sponsored study to evaluate the effects of opioids and benzodiazepines on all-cause mortality in veterans (including suicide) and quantify the effects of opioid and benzodiazepine prescribing on the risk of death among veterans who received VA care between 2007 and 2019.
-
Veterans are an impacted community with a more challenging status quo than other communities and suffer high rates of chronic pain and co-morbidities. The loss of life among veterans prescribed opiates for chronic pain is staggering. Veterans impacted by opioids face a lifelong struggle.
Pain-relief medications, including controlled substances, are the most frequent form of medication used in suicide attempts via overdose. Service members are prescribed narcotic painkillers while serving in the military at three times the rate of civilians.
An internal briefing from the Walter Reed’s Alcohol and Substance Abuse Program disclosed that nearly half of the soldiers in the Warrior Transition Units had narcotic prescriptions at the end of 2009, with roughly the same number having TBI and/or PTSD.
In 2010, Army Surgeon General Lt. Gen. Eric Schoomaker estimated almost 14% of the force had been prescribed some form of opiate drug.
By 2011, an estimated 25–35% of combat-wounded soldiers in WTUs experienced addiction or dependence on prescription drugs, particularly those provided in combat settings or military hospitals.
Madigan Army Medical Center Pychiatrist Dr. Russell Hicks indicated 5% of the troops had two or more active prescriptions for opiates; 60% of the soldiers with PTSD seen in the Intensive Outpatient Program had a co-occurring substance use disorder.
Pain is the most frequent presenting complaint reported by service members in community and primary care settings, including nearly half of returning combat veterans signing into the VA with pain-related diagnoses from 2005–2008.
A VA study analyzing data on 123,946 veterans who received VA care in 2004–2005 and received opioids for non-cancer chronic pain found those being prescribed the highest doses were more than twice as likely to die by suicide between 2004–2009 compared to those with the lowest doses.
While opioid therapy was once largely in the domain of cancer and pain specialists, up to 80% of opioids were prescribed in VA primary care by 2010; the majority of long-acting opioids were prescribed for non-cancer pain.
Patients initiating therapy with long-acting opioids were more than twice as likely to overdose compared with persons initiating therapy with short-acting opioids, particularly within the first two weeks after initiation.
More than half of all veterans receiving care at VHA for chronic pain present with co-morbid mental health conditions. These veterans have a significantly greater risk of being prescribed the highest dose, highest risk opioid therapy by VA clinicians and for experiencing adverse outcomes.
Veterans with PTSD experiencing chronic pain were more than twice as likely to be prescribed opioids.
Veterans with PTSD and a history of substance use disorder were four times as likely to be prescribed opioids.
High dose, high risk opioid therapies had the worst outcomes for veterans with co-morbid mental health conditions, particularly those with PTSD. Around 75% of Vietnam veterans with PTSD have a co-occurring substance use disorder.
Veterans with co-morbid mental health conditions were the most likely to obtain early refills, to be prescribed higher doses, take opioids longer, and to receive concurrent opioid, sedative, and/or hypnotics prescriptions.
Long-term opioid therapy is associated with significant and well-known risks, particularly in vulnerable individuals experiencing chronic pain and co-morbid mental health and/or post-concussive conditions.
Despite the risks and lack of evidence supporting the efficacy of long-term opioid therapy, opiate prescription rates at VA rose by 270% between 2001 and 2013. Of the more than a half million veterans receiving chronic or long-acting opioid therapy from the VA in 2016, more than a third were receiving sedatives concurrently; and
Concurrent opioid and benzodiazepine prescription rates for veterans with PTSD in the VA were above 30%, despite the risk of their death from drug overdose increasing in a dose-response fashion.
As part of the 2013 Opioid Safety Initiative, VA stated its intent to leverage its electronic health record to identify patients with one or more risk factors, as well as providers whose prescribing practices are misaligned with medical evidence or best practices, in order to intervene.
With complete data, the VA’s electronic health record can alert providers of best practices, recommend evidence-based courses of treatment, and flag high-risk situations or potential violations of best practices, guidelines, and policy in order to improve quality and oversight and embed learning in care.
Matching of PDMP data to treatment records within the VA’s electronic health record has potential to improve care and patient safety while also opening up new opportunities for research, maximizing the value of the data at the point of care and developing best practices in data integration that can be applied across federal systems.
The VA has not yet leveraged the use of clinical alerts across the VA healthcare system to further mitigate the risk of potentially inappropriate prescribing and co-prescribing of CNS-acting medications and enhance patient safety and informed consent.
-
VA researchers have evaluated the impacts of veterans’ being prescribed multiple central nervous system (CNS) acting medications in multiple populations, noting that increases in the quantities prescribed have coincided with increases in overdoses and suicide-related behaviors.
The researchers found past DoD reports of “potentially problematic use of [CNS-acting] drugs,” including a review of suicide-related events conducted by the Army Institute of Public Health that found in a review that at least one CNS-acting medication was prescribed in the year prior to:
90% of suicide attempts;
87% of suicidal ideation events, and
46% of suicide deaths.
TRICARE data from 2005–2011 reportedly demonstrated a shift in prescribing practices with a:
1,083% increase in use of antipsychotics (vs. a 22% increase within the civilian population);
996% increase in use of sedating anticonvulsants;
713% increase in use of benzodiazepines; and
682% increase in use of psychoactive medications.
In 2015, DoD’s Medical Command issued Policy Memorandum 15-039 to provide guidance on the management of polypharmacy involving psychotropic medications and CNS depressants specifically with the goal of reducing adverse events and optimizing the health of service members and families receiving care.
In 2016, VA researchers examined experiences of more than 300,000 OIF/OEF veterans who received VA healthcare between 2009–2011. More than 8% were prescribed five or more CNS-acting drugs in 2011. CNS polypharmacy may independently increase the risk of overdose and suicide-related behavior. VA HSR&D released a Publication Brief about the findings here.
CNS polypharmacy was independently associated with documented overdose and suicide-related behaviors. OIF/OEF veterans with PTSD, depression, and TBI; women veterans; and veterans between ages 31–50 were more likely to have CNS polypharmacy. This may be a risk factor that could be used to “trigger” the evaluation of veterans’ care in order to decrease their risk of death.
-
In 2019, VA researchers evaluated menopausal symptoms and higher risk opioid prescribing. In a national sample of more than 100,000 women veterans aged 45–64 with chronic pain, menopausal symptoms were associated with potentially risky long-term opioid prescribing patterns, independent of other risk factors. Within this national sample, VA researchers found:
13% were prescribed high-dose long-term opioids;
35% were co-prescribed long-term opioids and CNS depressants; and
51% were prescribed long-term opioids.
The 17% of women veterans with documented menopausal symptoms were more likely to be prescribed high-dose long-term opioids, long-term opioids, and to have polypharmacy with long-term opioids co-prescribed with CNS depressants (sedative-hypnotics, gabapentin/ pregabalin, or muscle relaxants).
In 2022, VA researchers evaluated long-term psychoactive medications, polypharmacy, and risk of suicide and unintended overdose death in a national sample of more than 150,000 midlife and older women veterans. Long-term prescribing of psychoactive medications and psychoactive polypharmacy predicted their risk of suicide and/or overdose death above and beyond other factors:
Long-term opioids and benzodiazepines were both associated with death by suicide.
Opioids, benzodiazepines, sedative-hypnotics, antidepressants, antipsychotics, and antiepileptics were associated with unintended overdose death.
Polypharmacy with three or more psychoactive medications was associated with a more than two-fold increased risk of both suicide and unintended overdose death.
-
Benzodiazepines are contraindicated with PTSD. Long-term use of benzodiazepines can increase symptoms of anxiety and depression. Women are more likely to be inappropriately prescribed benzodiazepines.
The VA has worked to de-implement benzodiazepine prescribing for PTSD, resulting in a decrease from over 31% in 2009 to just under 11% in 2019. The largest decreases were accounted for by new patients with PTSD not being prescribed benzodiazepines, as opposed to tapering and discontinuation among patients who were already prescribed benzodiazepines for PTSD.
From 2009 to 2019, the proportion of older veterans inappropriately prescribed benzodiazepines increased for both new and existing patients. The VA has not implemented clinical alerts within its electronic health record to mitigate risks of inappropriate prescribing at the point of service.
VA offers information about benzodiazepines here. In order to educate patients about the risks, VA published the pamphlet Benzodiazepines & PTSD: Do you know about this risky combination?.
In September 2020, the FDA updated the Boxed Warning for benzodiazepines to address serious risks of abuse, addiction, physical dependence, and withdrawal that may result in overdose or death. Risk is especially high when benzodiazepines are combined with opioids, alcohol, or illicit drugs – even when taken at recommended doses – even over the course of only days/weeks.
In February 2023, a committee of the National Academies of Sciences, Engineering, and Medicine began a VA-sponsored study to evaluate the effects of opioids and benzodiazepines on all-cause mortality in veterans (including suicide) and quantify the effects of opioid and benzodiazepine prescribing on the risk of death among veterans who received VA care between 2007 and 2019.
-
Akathisia may occur when stopping, starting, or changing the dosage or type of certain medications, and it may have a delayed onset. Akathisia is characterized by a feeling of inner restlessness and a compelling need or urge to be in constant movement (fidgeting, rocking, pacing, etc).
Symptoms are often overlooked or mistaken as signs of new or worsening agitation, depression, or anxiety. It may be wrongly treated by raising the dose or adding new drugs as a result. It is important to learn about the causes and symptoms of akathisia to ensure it is promptly identified.
Patients with akathisia should be closely monitored due to suicide risk. Inner restlessness is experienced as distressing and may be expressed as impatience, apprehension, dysphoria, irritation, anger, rage, tension, confusion, fear, vague somatic complaints, dyspnea, or difficulty concentrating.
Other prominent symptoms may include exacerbation of hallucinations or delusions, manic activity, disruptive behavior, panic attacks, acting out, or self-destructive behaviors such as head banging. Such symptoms may be attributed to an underlying condition and/or mask akathisia.
Akathisia is most commonly understood and recognized in relation to the prescription of antipsychotic medications, but it can occur with medications prescribed for acne, depression, asthma, nausea, anxiety, malaria, insomnia, smoking cessation, high blood pressure, and others.
Akathisia has also been found more recently to occur as an adverse effect of calcium channel blockers, antiemetics, anti-vertigo drugs, and sedatives used in anesthesia. It may also occur with cocaine, methamphetamine, MDMA, ecstasy, and GHB.
People with any history of TBI may have an elevated suicide risk. TBI may also lead to akathisia. Other medical issues that may increase the risk for experiencing akathisia include hyperthyroidism, renal impairment, diabetes, iron deficiency anemia, Parkinson’s disease, and peripheral neuropathy.
Community Resources for Akathisia
The Medication-Induced Suicide Prevention and Education Foundation (MISSD) offers educational materials and a training with CE credit focused on recognizing akathisia. MISSD works to raise awareness of medication-induced suicide.
The Inner Compass Initiative offers information and a Help Hub for people having a psychiatric drug withdrawal journey and Quick Tips for coping with akathisia.
The Akathisia Alliance offers general information about benzodiazepines and akathisia for clinicians, family, and friends.
The Benzodiazepine Information Coalition offers resources and information about akathisia and benzodiazepines, including Benzodiazepines: How They Work and How To Withdraw (ie, “The Ashton Manual”).
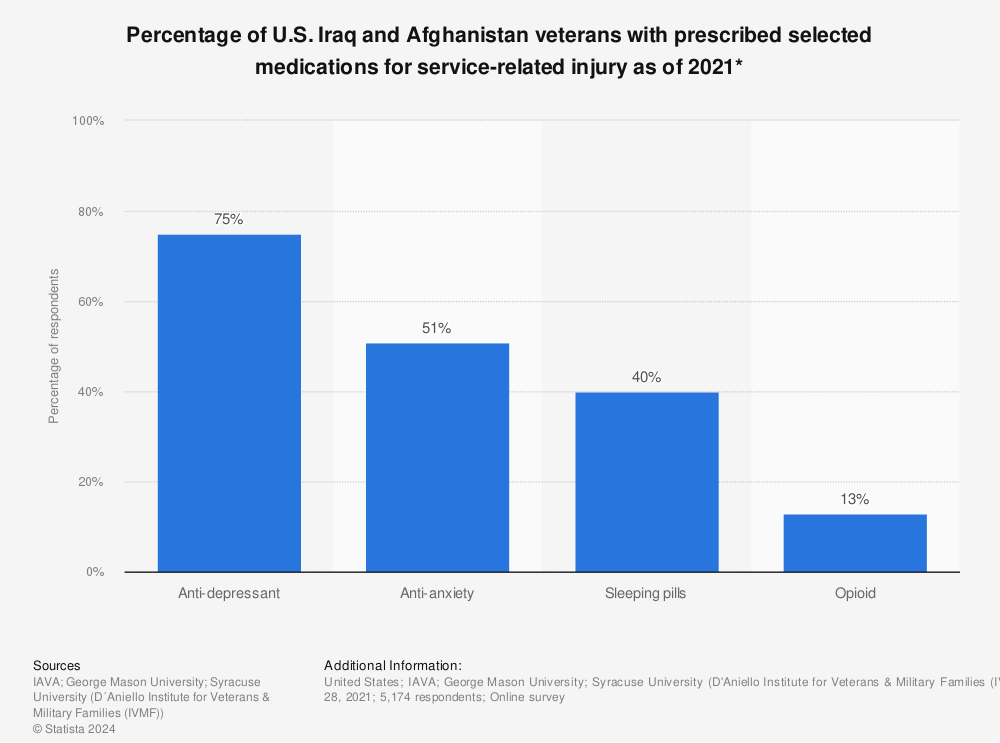
Iraq and Afghanistan Veterans of America’s annual survey of 5,174 veterans in 2021 asked if they had been prescribed or were currently taking prescription medications for service-connected injuries. Many medications can be harmful when used with alcohol or other substances, increasing the risk of serious side effects, unintentional overdose, and death.
In 2023, RAND published A Summary of Veteran-Related Statistics drawing from public nationally representative datasets demonstrating that veterans of all ages were more likely than nonveterans to get treatment for alcohol and substance use.
Only 2.3 percent of post 9/11 and 1.2 percent of pre 9/11 era veterans reported receiving treatment for alcohol or drug use in the past year and 36.5 percent of post 9/11 and 19.9 percent of pre 9/11 era veterans reported binge drinking in the past month.
“Obtaining prompt access to services is critical not only during times of crisis,” the 2023 VA National Suicide Prevention Report notes, “but when first initiating treatment, and in a sustained manner to complete a full episode of care.”
-
The HeartCore Collective is a healing community committed to creating spaces that foster honest dialogues about our modern mental health care systems and we are working to empower individuals on their healing journeys with education, resources, and support so they can make informed choices about their mental health. We are dedicated to providing person-centered holistic wellness and psychiatric drug withdrawal support.
By taking a non-medical and nonpathologizing approach, we focus on self-help, compassionately guiding individuals on their healing journeys. As informed peers who know this path well we provide evidence- and lived experience-based resources and tools to help others find their way forward. Our approach draws from the emerging field of deprescribing sciences and psychiatry and the shared wisdom from individuals with lived experience.
This is a holistic health collective that centers trauma-informed care with lifestyle interventions in order to create a new paradigm and existence for a community that has been historically overlooked and underrecognized. In this healing community, we get to the heart of what’s happening first because that’s what matters most.
Operation Deep Dive™
America’s Warrior Partnership’s Operation Deep Dive™ study currently encompasses five years of death data corroborated by the DoD from Massachusetts and seven other states. OpDD™ acquired state-wide death records for Massachusetts in 2020, which were prepared and delivered to the DoD for Phase I verification.
-
The goal of AWP’s OpDD™ research is to:
identify current/former service members with the highest probability of dying prematurely at a national/state/local level by correlating state death record data to detailed military experiences shared by DoD;
identify community environments that contribute to lower or higher premature deaths (ie, overdose, asphyxiation, accidental gunshot, drowning, suicide by law enforcement, or high-speed, single-driver accident) through qualitative interviews with friends, families, and co-workers to re-construct the deceased veteran’s last year;
identify the impact of adverse disciplinary actions on the premature death of current and former service members; and
use the findings to develop national/state/local suicide and overdose prevention strategies and identify possible changes in clinical and public health practice for former service members.
OpDD™ uses the definition of Self Injury Mortality (SIM) cited by CDC and NIH, merging registered/known suicides with accidents and undetermined deaths aligned with self-harm or suicidal behavior, which have been attributed predominantly to overdose deaths. From 2014–18, the suicide rate was 37% greater than reported by VA; states undercounted deaths at an error rate of 25%.
Refer to the OpDD™ Methodology Report for more information on the study design, methodology, data, and limitations. State Data Sheets are expected to be released. OpDD™ Annual Reports are available for 2019, 2020, 2021, and 2023.
In 2022, AWP released Summary of Interim Report with a finding that found veterans in the eight states analyzed with less than 3 years of service has the greatest risk for suicide and overdose death.
Based on the 2023 Annual Report, data from the Massachusetts death certificates was prepared and sent to DoD to be linked to military records in October 2023.
AWP is seeking relatives, loved ones, friends, and co-workers of former service members who died by suicide or self-injury, including death by overdose, asphyxiation, accidental gunshot, drowning, suicide by law enforcement interaction, or high-speed, single-driver accidents, within the past 24 months for private interviews. Click here for more information.
Veterans Harm Reduction Summit
The Veterans Collaborative and Grunt Style Foundation hosted the first Massachusetts Veterans Harm Reduction Summit on December 11th in collaboration with VFW Department of Massachusetts, Mad in America, HeartCore Collective, Irreverent Warriors and 22Mohawks at Boston Police VFW Post 1018, learning from experts alongside impacted veterans and survivors exploring safe prescribing and deprescribing and reviewing the available public health data involving military and veteran suicide and overdose deaths in Massachusetts and beyond. Check out HARMREDUCTION.vet to learn more.